
IBS Diagnosis, Facts, and Treatment Options
Written by Colleen MacKay, RD; edited by Brooke Bulloch, RD
Irritable Bowel Syndrome (IBS) can affect people of all ages. It is estimated that 13-20% of Canadians live with IBS. Despite this massive prevalence, there is a lot that people don’t know about the condition or how to manage it. I’m Colleen MacKay, and as a gastrointestinal dietitian who supports clients with gut function, some of the most common questions I get are: “what is wrong with my gut?”, “what is causing my symptoms?” and “how can I improve my quality of life?”. In this blog post, I’m going to cover what IBS is, how it’s diagnosed, possible symptom triggers, and treatment options.
What is IBS?
IBS is a disorder of the gut-brain interaction. This means that the gut (stomach, small intestine and/or large intestine) is not functioning properly in relation to central nervous system processing. So a gastroscopy won’t show inflammation, ulcers, or structural issues as seen in people with celiac disease, Crohn’s or Colitis. Instead, people with IBS regularly experience real symptoms such as:
- Abdominal pain or cramping
- Abdominal bloating and distension
- Gas
- Diarrhea and/or constipation.
How Is ibs diagnosed?
The Rome Foundation diagnostic criteria for IBS includes:
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool
* Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.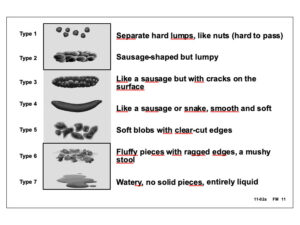
Does IBS increase my risk for other health issues?
An important distinction between IBS and other bowel diseases is that IBS does not damage the structure of the gut. It doesn’t increase the risk for colorectal cancer or surgery, or decrease life expectancy. However, IBS affects an individual’s quality of life. People with IBS experience absences from work or school, and often struggle with self-blame, guilt, anger, and social isolation.
What Causes IBS Symptoms?
Before discussing the cause of IBS symptoms, we first need to understand what “normal” digestion looks like. After a food is eaten, it will move through all parts of the digestive system – mouth, esophagus, stomach, small intestine, and large intestine – being broken down along the way. This is done through motion such as chewing, squeezing and mixing, and the action of digestive juices. Bacteria in the large intestine also help with digestion. As food is broken down, nutrients that the body needs are extracted and absorbed into the bloodstream, and the waste left behind results in a bowel movement. This whole process is controlled by hormones and nerves that communicate not only within the gut, but also back and forth along the gut-brain-axis.
For people with IBS, this process does not work correctly. Two of the more common disruptions causing symptoms relate to: 1) issues breaking down certain types of foods (ie. FODMAP-containing foods); and/or 2) an oversensitive, over-reactive gut (called visceral hypersensitivity).
what are FODMAPs?
Research investigating the relationship between diet and IBS has focused on FODMAPs
Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
These are short-chain carbohydrates and sugar alcohols that trigger symptoms in people with IBS. This is because they pull extra water into the small intestine leading to diarrhea and cramping. FODMAPs are also fermented in the large intestine leading to excess gas production, distention, and pain. Decreasing the intake of high FODMAP foods has been shown to reduce symptoms in 3 out of 4 people with IBS.
People are often surprised to hear that many high FODMAP foods are everyday, nourishing foods. This does not mean that these foods are “bad” for you, it just means that your body may be having trouble breaking them down.
The low FODMAP diet is a 3-phase, therapeutic diet that should not exceed 6 weeks in duration. It’s recommended to work with an experienced dietitian.
what is visceral hypersensitivity and how do I know if I have it?
Visceral hypersensitivity (VH) is a complex interaction between the nerves of the gut and the nerves in the brain (referred to as the gut-brain-axis). It is defined as experiencing pain in the inner organs. People with visceral hypersensitivity have a more sensitive digestive system that reacts more strongly to the pressure put on the bowel by gas produced during digestion.
While the stimulation of digestion should not be painful, in IBS the oversensitive nerves of the gut overreact and send signals to the brain that something is wrong. This results in the brain identifying the sensation of pain, cramping and even bloating. The brain might also tell the bowel to change the speed of contraction, resulting in either diarrhea or constipation (or both!). It is unknown why some people have a more sensitive gut, but one theory is that hypersensitivity can start after the gut is irritated by a virus, illness or injury.
VH is a new diagnosis and we don’t know how common it is. There is no set diagnostic criteria for VH.
There are many factors that contribute to IBS symptoms, and because of this there are many different treatment options available, including:
- Diet and lifestyle options such as the low FODMAP diet phases
- Nutritional supplements
- Herbal remedies
- Medications
- Psychological therapies (e.g. cognitive behavioural therapy or hypnotherapy).
Most often a combination of treatment options help with symptom relief. If you are interested in navigating your IBS symptoms, your triggers, dietary treatment options, and long-term management of IBS, book a consultation with myself or Brooke to learn more.
LET'S STAY IN TOUCH
Join our mailing list
Join our newsletter for more non-diet content including practical nourishment, recipes, nutrition myth-busting, and weight inclusive well-being.

Curiosity, self-compassion, food peace. Nutrition assessment, planning, and monitoring + food relationship counseling.
Food to Fit Locations:
#203, 2445 Broad Street
Regina, Saskatchewan
1124 8th Street East
Saskatoon, Saskatchewan





